Cardiac imaging
| Cardiac imaging | |
|---|---|
| Diagnostics | |
| ICD-10-PCS | |
| MeSH | D057791 |
Cardiac imaging techniques include coronary catheterization, echocardiogram, Intravascular ultrasound, Cardiac PET scan, Cardiac CT scan and Cardiac MRI.
Indications
A physician may recommend cardiac imaging to support a diagnosis of a heart condition.
Medical specialty professional organizations discourage the use of routine cardiac imaging during pre-operative assessement for patients about to undergo low or mid-risk non-cardiac surgery because the procedure carries risks and is unlikely to result in the change of a patient's management.[1] Stress cardiac imaging is discouraged in the evaluation of patients without cardiac symptoms or in routine follow-ups.[2]
Coronary catheterization

Coronary catheterization uses pressure monitoring and blood sampling through a catheter inserted into the heart through blood vessels in the leg to determine the functioning of the heart, and, following injections of radiocontrast dye, uses X-ray fluoroscopy, typically at 30 frames per second, to visualize the position and volume of blood within the heart chambers and arteries. Coronary angiography is used to determine the patency and configuration of the coronary artery lumens.
Echocardiogram

Transthoracic echocardiogram uses ultrasonic waves for continuous heart chamber and blood movement visualization. In recent times, it has become one of the most commonly used tools in diagnosis of heart problems, as it allows non-invasive visualization of the heart and the blood flow through the heart, using a technique known as Doppler.
Transoesophageal echocardiogram uses a specialized probe containing an ultrasound transducer at its tip is passed into the patient's esophagus. It is used in diagnosis of various thoracic defects or damage, i.e. heart and lung imaging. It has some advantages and disadvantages over thoracic or intravasular ultrasound.
Intravascular ultrasound

Intravascular ultrasound, also known as a percutaneous echocardiogram is an imaging methodology using specially designed, long, thin, complex manufactured catheters attached to computerized ultrasound equipment to visualize the lumen and the interior wall of blood vessels.
FFR
Specifically examines the flow velocity within suspected ischemic vessels that may require PCI, establishes interventional guidelines.
Positron emission tomography
Positron emission tomography (PET), an imaging methodology for positron emitting radioisotopes. PET enables visual image analysis of multiple different metabolic chemical processes and is thus one of the most flexible imaging technologies. Cardiology uses are growing very slowly due to technical and relative cost difficulties. Most uses are for research, not clinical purposes. Appropriate radioisotopes of elements within chemical compounds of the metabolic pathway being examined are used to make the location of the chemical compounds of interest visible in a PET scanner constructed image.
Computed tomography angiography
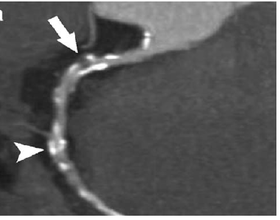
Computed tomography angiography (CTA), an imaging methodology using a ring-shaped machine with an X-Ray source spinning around the circular path so as to bathe the inner circle with a uniform and known X-Ray density. Cardiology uses are growing with the incredible developments in CT technology. Currently, multidetector CT, specially the 64 detector-CT are allowing to make cardiac studies in just a few seconds (less than 10 seconds, depending on the equipment and protocol used). These images are reconstructed using algorithms and software. Great development and growth will be seen in the short term, allowing radiologists to diagnose cardiac artery disease without anesthesia and in a non-invasive way.
Magnetic resonance imaging

Magnetic resonance imaging (originally called nuclear magnetic resonance imaging), an imaging methodology based on aligning the spin axis of nuclei within molecules of the object being visualized using both powerful superconducting magnets and radio frequency signals and detectors. Cardiology uses are growing, especially since MRI differentiates soft tissues better than CT and allows for comprehensive exams including the quantitative assessment of size, morphology, function, and tissue characteristics in one single session. Current implementations for Cardiology uses are sometimes limited by lengthy protocols, claustrophobia and contraindications based on some complex metallic implants (pacemakers, defibrillators, insulin pumps), while artificial valves and coronary stents are generally not problematic. Image quality can be reduced by the continuous movement of heart structures. There is a promising future in cardiac MRI by more efficient scans, increasing availability of scanners and more widespread knowledge about its clinical application.
References
- ↑ American Society of Nuclear Cardiology, "Five Things Physicians and Patients Should Question" (PDF), Choosing Wisely: an initiative of the ABIM Foundation, American Society of Nuclear Cardiology, retrieved August 17, 2012, citing
- Hendel, R. C.; Berman, D. S.; Di Carli, M. F.; Heidenreich, P. A.; Henkin, R. E.; Pellikka, P. A.; Pohost, G. M.; Williams, K. A.; American College of Cardiology Foundation Appropriate Use Criteria Task Force; American Society of Nuclear Cardiology; American College Of, R.; American Heart, A.; American Society of Echocardiology; Society of Cardiovascular Computed Tomography; Society for Cardiovascular Magnetic Resonance; Society Of Nuclear, M. (2009). "ACCF/ASNC/ACR/AHA/ASE/SCCT/SCMR/SNM 2009 Appropriate Use Criteria for Cardiac Radionuclide Imaging". Journal of the American College of Cardiology. 53 (23): 2201–2229. doi:10.1016/j.jacc.2009.02.013. PMID 19497454.
- Fleisher, L. A.; Beckman, J. A.; Brown, K. A.; Calkins, H.; Chaikof, E. L.; Fleischmann, K. E.; Freeman, W. K.; Froehlich, J. B.; Kasper, E. K.; Kersten, J. R.; Riegel, B.; Robb, J. F.; Smith Jr, S. C.; Jacobs, A. K.; Adams, C. D.; Anderson, J. L.; Antman, E. M.; Buller, C. E.; Creager, M. A.; Ettinger, S. M.; Faxon, D. P.; Fuster, V.; Halperin, J. L.; Hiratzka, L. F.; Hunt, S. A.; Lytle, B. W.; Nishimura, R.; Ornato, J. P.; Page, R. L.; Riegel, B. (2007). "ACC/AHA 2007 Guidelines on Perioperative Cardiovascular Evaluation and Care for Noncardiac Surgery". Journal of the American College of Cardiology. 50 (17): e159–e241. doi:10.1016/j.jacc.2007.09.003. PMID 17950140.
- ↑ American College of Cardiology (September 2013), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation, American College of Cardiology, retrieved 10 February 2014