Endocarditis
| Endocarditis | |
|---|---|
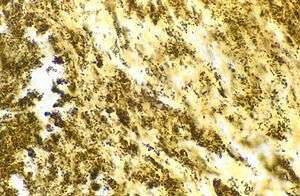 | |
| Bartonella henselae bacilli in cardiac valve of a patient with blood culture-negative endocarditis. The bacilli appear as black granulations. | |
| Classification and external resources | |
| Specialty | Cardiology, infectious disease |
| ICD-10 | I33 |
| ICD-9-CM | 421 |
| DiseasesDB | 4224 |
| MedlinePlus | 001098 |
| eMedicine | emerg/164 med/671 ped/2511 |
| Patient UK | Endocarditis |
| MeSH | D004696 |
Endocarditis is an inflammation of the inner layer of the heart, the endocardium. It usually involves the heart valves. Other structures that may be involved include the interventricular septum, the chordae tendineae, the mural endocardium, or the surfaces of intracardiac devices. Endocarditis is characterized by lesions, known as vegetations, which is a mass of platelets, fibrin, microcolonies of microorganisms, and scant inflammatory cells.[1] In the subacute form of infective endocarditis, the vegetation may also include a center of granulomatous tissue, which may fibrose or calcify.[2]
There are several ways to classify endocarditis. The simplest classification is based on cause: either infective or non-infective, depending on whether a microorganism is the source of the inflammation or not. Regardless, the diagnosis of endocarditis is based on clinical features, investigations such as an echocardiogram, and blood cultures demonstrating the presence of endocarditis-causing microorganisms. Signs and symptoms include: fever, chills, sweating, malaise, weakness, anorexia, weight loss, splenomegaly, flu-like feeling, cardiac murmur, heart failure, petechia of anterior trunk, Janeway's lesions, etc.
Cause
Infective
Since the valves of the heart do not receive any dedicated blood supply, defensive immune mechanisms (such as white blood cells) cannot directly reach the valves via the bloodstream. If an organism (such as bacteria) attaches to a valve surface and forms a vegetation, the host immune response is blunted. The lack of blood supply to the valves also has implications on treatment, since drugs also have difficulty reaching the infected valve.
Normally, blood flows smoothly past these valves. If they have been damaged (from rheumatic fever, for example) the risk of bacteria attachment is increased.[2]
Rheumatic fever is common worldwide and responsible for many cases of damaged heart valves. Chronic rheumatic heart disease is characterized by repeated inflammation with fibrinous resolution. The cardinal anatomic changes of the valve include leaflet thickening, commissural fusion, and shortening and thickening of the tendinous cords.[3] The recurrence of rheumatic fever is relatively common in the absence of maintenance of low dose antibiotics, especially during the first three to five years after the first episode. Heart complications may be long-term and severe, particularly if valves are involved. While rheumatic fever since the advent of routine penicillin administration for Strep throat has become less common in developed countries, in the older generation and in much of the less-developed world, valvular disease (including mitral valve prolapse, reinfection in the form of valvular endocarditis, and valve rupture) from undertreated rheumatic fever continues to be a problem.[4]
In an Indian hospital between 2004 and 2005, 4 of 24 endocarditis patients failed to demonstrate classic vegetation. All had rheumatic heart disease and presented with prolonged fever. All had severe eccentric mitral regurgitation. (One had severe aortic regurgitation also.) One had flail posterior mitral leaflet.[5]
Non-infective
Nonbacterial thrombotic endocarditis (NBTE), also called marantic endocarditis is most commonly found on previously undamaged valves.[2] As opposed to infective endocarditis, the vegetations in NBTE are small, sterile, and tend to aggregate along the edges of the valve or the cusps.[2] Also unlike infective endocarditis, NBTE does not cause an inflammation response from the body.[2] NBTE usually occurs during a hypercoagulable state such as system-wide bacterial infection, or pregnancy, though it is also sometimes seen in patients with venous catheters.[2] NBTE may also occur in patients with cancers, particularly mucinous adenocarcinoma[2] where Trousseau syndrome can be encountered. Typically NBTE does not cause many problems on its own, but parts of the vegetations may break off and embolize to the heart or brain, or they may serve as a focus where bacteria can lodge, thus causing infective endocarditis.[2]
Another form of sterile endocarditis is termed Libman–Sacks endocarditis; this form occurs more often in patients with lupus erythematosus and is thought to be due to the deposition of immune complexes.[2] Like NBTE, Libman-Sacks endocarditis involves small vegetations, while infective endocarditis is composed of large vegetations.[2] These immune complexes precipitate an inflammation reaction, which helps to differentiate it from NBTE. Also unlike NBTE, Libman-Sacks endocarditis does not seem to have a preferred location of deposition and may form on the undersurfaces of the valves or even on the endocardium.[2]
Diagnostics
Examination of suspected infective endocarditis includes a detailed examination of the patient, complete history taking, and especially careful cardiac auscultation, various blood tests, ECG, cardiac ultrasound (echocardiography). Analysis of blood helps reveal the typical signs of inflammation (increased erythrocyte sedimentation rate, leukocytosis). Two or more separate blood cultures are normally drawn. Negative blood cultures, however, do not exclude the diagnosis of infective endocarditis. Echocardiography (through the anterior chest wall or transesophageal), plays a decisive role in the diagnosis by reliably establishing the presence of microbial vegetation and the degree of valvular dysfunction affecting the pumping function of the heart.[6]
References
- ↑ Kasper DL, Braunwald E, Fauci AS, Hauser S, Longo DL, Jameson JL (May 2005). Harrison's Principles of Internal Medicine. McGraw-Hill. pp. 731–40. ISBN 0-07-139140-1. OCLC 54501403.
- 1 2 3 4 5 6 7 8 9 10 11 Mitchell RS, Kumar V, Robbins SL, Abbas AK, Fausto N (2007). Robbins Basic Pathology (8th ed.). Saunders/Elsevier. pp. 406–8. ISBN 1-4160-2973-7.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease. St. Louis, Mo: Elsevier Saunders. ISBN 0-7216-0187-1.
- ↑ NLM/NIH: Medline Plus Medical Encyclopedia: Rheumatic fever
- ↑ S Venkatesan; et al. (Sep–Oct 2007). "Can we diagnose Infective endocarditis without vegetation ?". Indian Heart Journal. 59 (5).
- ↑ http://medusanews.com/diseases-and-conditions/cardiology/endocarditis.html
External links
Endocarditis at DMOZ