Intracoronary optical coherence tomography
| Intracoronary Optical coherence tomography | |
|---|---|
| Intervention | |
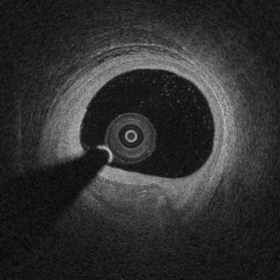 Example of Intracoronary Optical Coherence Tomography (OCT) image of atherosclerosis. Between 6 and 8 o'clock it is possible to observe a fibrocalcific Atherosclerotic plaque. |
Intracoronary optical coherence tomography (OCT) (or, more generally, intravascular optical coherence tomography, IVOCT), is an endoscopic based application of optical coherence tomography. Analogous to IVUS, intracoronary OCT uses a catheter to deliver and collect near infrared light (e.g., 1,300 nm) to create cross-sectional images images of artery lumen. Intracoronary OCT creates images at a resolution of approximately 15 micro-meters, an order of magnitude improved resolution with respect to IVUS and x-ray coronary angiogram.[1][2]
Methods
State-of-the-art intracoronary optical coherence tomography typically uses a swept-source laser to acquire OCT images at high-speed of approximately 80,000 kHz (A-scan lines per second) to complete acquisition of a 3D OCT volume of a coronary segments in a few-seconds.[3]
Clinical applications
Approximately 100,000 intracoronary optical coherence tomography procedures are performed every year and its adoption is rapidly growing at a rate of ~20% every year.[4] Evidence showed that intracoronary OCT can be used to optimize percutaneous coronary intervention (PCI) to treat myocardial infarction and that OCT imaging influence physician decision in >50% of the cases.[5]
Assessment of artery lumen morphology is the cornerstone of intravascular imaging criteria to evaluate disease severity and guide intervention. The high-resolution of OCT imaging allows to assess with high accuracy vessel lumen area, wall microstructure, intracoronary stent apposition and expansion. OCT has an improved ability with respect to IVUS to penetrate and delineate calcium in the vessel wall that makes it well suited to guide complex interventional strategies in vessels with superficial calcification. OCT has the capability of visualize coronary plaque erosion and fibrotic caps overlying atheromas.[2]
Safety
Safety of intravascular imaging, including intracoronary OCT and intravascular ultrasound, has been investigated by several studies. Recent clinical trials reported a very low rate of self-limiting, minor complications on over 3,000 patients where in all cases no harm or prologation of hospital stay was observed. Intracoronary optical coherence tomography was demonstrates to be safe among heterogeneous groups of patients presenting varying clinical setting.[6]
References
- ↑ Bezerra, Hiram G.; Costa, Marco A.; Guagliumi, Giulio; Rollins, Andrew M.; Simon, Daniel I. (2009). "Intracoronary Optical Coherence Tomography: A Comprehensive Review". JACC: Cardiovascular Interventions. 2 (11): 1035–1046. doi:10.1016/j.jcin.2009.06.019. ISSN 1936-8798.
- 1 2 Tearney, Guillermo J.; Regar, Evelyn; Akasaka, Takashi; Adriaenssens, Tom; Barlis, Peter; Bezerra, Hiram G.; Bouma, Brett; Bruining, Nico; Cho, Jin-man; Chowdhary, Saqib; Costa, Marco A.; de Silva, Ranil; Dijkstra, Jouke; Di Mario, Carlo; Dudeck, Darius; Falk, Erlin; Feldman, Marc D.; Fitzgerald, Peter; Garcia, Hector; Gonzalo, Nieves; Granada, Juan F.; Guagliumi, Giulio; Holm, Niels R.; Honda, Yasuhiro; Ikeno, Fumiaki; Kawasaki, Masanori; Kochman, Janusz; Koltowski, Lukasz; Kubo, Takashi; Kume, Teruyoshi; Kyono, Hiroyuki; Lam, Cheung Chi Simon; Lamouche, Guy; Lee, David P.; Leon, Martin B.; Maehara, Akiko; Manfrini, Olivia; Mintz, Gary S.; Mizuno, Kyiouchi; Morel, Marie-angéle; Nadkarni, Seemantini; Okura, Hiroyuki; Otake, Hiromasa; Pietrasik, Arkadiusz; Prati, Francesco; Räber, Lorenz; Radu, Maria D.; Rieber, Johannes; Riga, Maria; Rollins, Andrew; Rosenberg, Mireille; Sirbu, Vasile; Serruys, PatrickmW.J.C.; Shimada, Kenei; Shinke, Toshiro; Shite, Junya; Siegel, Eliot; Sonada, Shinjo; Suter, Melissa; Takarada, Shigeho; Tanaka, Atsushi; Terashima, Mitsuyasu; Troels, Thim; Uemura, Shiro; Ughi, Giovanni J.; van Beusekom, Heleen M.M.; van der Steen, Antonius F.W.; van Es, Gerrit-Ann; van Soest, Gijs; Virmani, Renu; Waxman, Sergio; Weissman, Neil J.; Weisz, Giora (2012). "Consensus Standards for Acquisition, Measurement, and Reporting of Intravascular Optical Coherence Tomography Studies". Journal of the American College of Cardiology. 59 (12): 1058–1072. doi:10.1016/j.jacc.2011.09.079. ISSN 0735-1097.
- ↑ S. H. Yun, G. Tearney, J. de Boer & B. Bouma (2004). "Pulsed-source and swept-source spectral-domain optical coherence tomography with reduced motion artifacts". Optics express. 12 (23): 5614–5624. PMID 19488195.
- ↑ Swanson, Eric (13 June 2016). "Optical Coherence Tomography: Beyond better clinical care: OCT's economic impact". BioOptics World. Retrieved 9 September 2016.
- ↑ Wijns, William; Shite, Junya; Jones, Michael R.; Lee, Stephen W.-L.; Price, Matthew J.; Fabbiocchi, Franco; Barbato, Emanuele; Akasaka, Takashi; Bezerra, Hiram; Holmes, David (2015). "Optical coherence tomography imaging during percutaneous coronary intervention impacts physician decision-making: ILUMIEN I study". European Heart Journal. 36 (47): 3346–3355. doi:10.1093/eurheartj/ehv367. ISSN 0195-668X.
- ↑ Johannes N. van der Sijde, Antonios Karanasos, Nienke S. van Ditzhuijzen, Takayuki Okamura, Robert-Jan van Geuns, Marco Valgimigli, Jurgen M. R. Ligthart, Karen T. Witberg, Saskia Wemelsfelder, Jiang Ming Fam, BuChun Zhang, Roberto Diletti, Peter P. de Jaegere, Nicolas M. van Mieghem, Gijs van Soest, Felix Zijlstra, Ron T. van Domburg & Evelyn Regar (2016). "Safety of optical coherence tomography in daily practice: a comparison with intravascular ultrasound". European heart journal cardiovascular Imaging. doi:10.1093/ehjci/jew037. PMID 26992420.