Pancreatic acinar metaplasia
Pancreatic acinar metaplasia, abbreviated PAM, is a common incidental histopathologic finding present in approximately 20-25% of patients undergoing an esophagogastroduodenoscopy.[1][2]
Significance
Studies are mixed on whether it is associated with pathology and symptoms.[2] There is some epidemiological evidence to suggest is associated with gastroesophageal reflux and Helicobacter gastritis.[1]
There is no evidence to suggest it is pre-neoplastic, like Barrett's esophagus.
Etiology
A slight increased incidence with age suggests, it is an acquired lesion,[1] as may be seen in a true metaplasia.
Histopathology
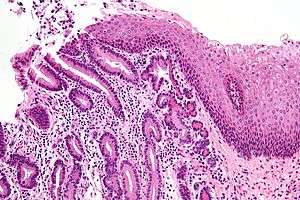
The histopathologic features of pancreatic acinar metaplasia are: (1) the presence of cell clusters that resembles a many-lobed "berry" (an acinus), with (2) cells that are histomorphologically identical to the glands of the exocrine pancreas.
See also
References
- 1 2 3 Johansson J, Håkansson HO, Mellblom L, et al. (March 2010). "Pancreatic acinar metaplasia in the distal oesophagus and the gastric cardia: prevalence, predictors and relation to GORD". J. Gastroenterol. 45 (3): 291–9. doi:10.1007/s00535-009-0161-4. PMID 20012917.
- 1 2 Wang HH, Zeroogian JM, Spechler SJ, Goyal RK, Antonioli DA (December 1996). "Prevalence and significance of pancreatic acinar metaplasia at the gastroesophageal junction". Am. J. Surg. Pathol. 20 (12): 1507–10. doi:10.1097/00000478-199612000-00010. PMID 8944044.