Pericarditis
| Pericarditis | |
|---|---|
|
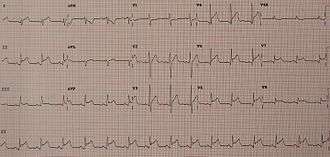
An ECG showing pericarditis. Note the ST elevation in multiple leads with slight reciprocal ST depression in aVR. | |
| Classification and external resources | |
| Specialty | Cardiology |
| ICD-10 | I01.0, I09.2, I30–I32 |
| ICD-9-CM | 420.0, 420.90, 420.91, 420.99, 423.1, 423.2 |
| DiseasesDB | 9820 |
| MedlinePlus | 000182 |
| eMedicine | med/1781 emerg/412 |
| MeSH | D010493 |
Pericarditis is inflammation of the pericardium (the fibrous sac surrounding the heart).[1] Symptoms typically include sudden onset of sharp chest pain. The pain may also be felt in the shoulders, neck, or back. It is typically better sitting up and worse with lying down or breathing deep. Other symptoms may include fever, weakness, palpitations, and shortness of breath.[2] Occasionally onset of symptoms is gradual.[1]
The cause of pericarditis is believed to be most often due to a viral infection.[3] Other causes include bacterial infections such as tuberculosis, uremic pericarditis, following a heart attack, cancer, autoimmune disorders, and chest trauma.[3][4] The cause often remains unknown.[3][1] Diagnosis is based on the chest pain, a pericardial rub, specific electrocardiogram (ECG) changes, and fluid around the heart.[5] Other conditions that may produce similar symptoms include a heart attack.[2]
Treatment in most cases is with NSAIDs and possibly colchicine. Steroids may be used if those are not appropriate.[5] Typically symptoms improve in a few days to weeks but can occasionally last months.[6] Complications can include cardiac tamponade, myocarditis, and constrictive pericarditis.[2][7] It is a less common cause of chest pain.[8] About 3 per 10,000 people are affected per year.[7] Those most commonly affected are males between the ages of 20 and 50. Up to 30% of those affected have more than one episode.[9]
Signs and symptoms
Substernal or left precordial pleuritic chest pain with radiation to the trapezius ridge (the bottom portion of scapula on the back), which is relieved by sitting up and bending forward and worsened by lying down (recumbent or supine position) or inspiration (taking a breath in), is the characteristic pain of pericarditis.[10] The pain may resemble the pain of angina pectoris or heart attack, but differs in that pain changes with body position, as opposed to heart attack pain that is pressure-like, and constant with radiation to the left arm and/or the jaw. Other symptoms of pericarditis may include dry cough, fever, fatigue, and anxiety. Due to similarity to myocardial infarction (heart attack) pain, pericarditis can be misdiagnosed as an acute myocardial infarction (a heart attack) solely based on the clinical data and so extreme suspicion on the part of the diagnostician is required. Acute myocardial infarction (heart attack) can also cause pericarditis, but the presenting symptoms often differ enough to warrant diagnosis. The following table organizes the clinical presentation of pericarditis:[10]
| Characteristic | Pericarditis | Myocardial infarction |
|---|---|---|
| Pain description | Sharp, pleuritic, retro-sternal (under the sternum) or left precordial (left chest) pain | Crushing, pressure-like, heavy pain. Described as "elephant on the chest." |
| Radiation | Pain radiates to the trapezius ridge (to the lowest portion of the scapula on the back) or no radiation. | Pain radiates to the jaw or left arm, or does not radiate. |
| Exertion | Does not change the pain | Can increase the pain |
| Position | Pain is worse in the supine position or upon inspiration (breathing in) | Not positional |
| Onset/duration | Sudden pain, that lasts for hours or sometimes days before a patient comes to the ER | Sudden or chronically worsening pain that can come and go in paroxysms or it can last for hours before the patient decides to come to the ER |
Physical examinations
The classic sign of pericarditis is a friction rub heard with a stethoscope on the cardiovascular examination usually on the lower left sternal border.[10] Other physical signs include a patient in distress, positional chest pain, diaphoresis (excessive sweating), and possibility of heart failure in form of pericardial tamponade causing pulsus paradoxus, and the Beck's triad of low blood pressure (due to decreased cardiac output), distant (muffled) heart sounds, and distension of the jugular vein (JVD).
Complications
Pericarditis can progress to pericardial effusion and eventually cardiac tamponade. This can be seen in patients who are experiencing the classic signs of pericarditis but then show signs of relief, and progress to show signs of cardiac tamponade which include decreased alertness and lethargy, pulsus paradoxus (decrease of at least 10 mmHg of the systolic blood pressure upon inspiration),low blood pressure (due to decreased cardiac index), (jugular vein distention from right sided heart failure and fluid overload), distant heart sounds on auscultation, and equilibration of all the diastolic blood pressures on cardiac catheterization due to the constriction of the pericardium by the fluid.
In such cases of cardiac tamponade, EKG or Holter monitor will then depict electrical alternans indicating wobbling of the heart in the fluid filled pericardium, and the capillary refill might decrease, as well as severe vascular collapse and altered mental status due to hypoperfusion of body organs by a heart that can not pump out blood effectively.
The diagnosis of tamponade can be confirmed with trans-thoracic echocardiography (TTE), which should show a large pericardial effusion and diastolic collapse of the right ventricle and right atrium. Chest X-ray usually shows an enlarged cardiac silhouette ("water bottle" appearance) and clear lungs. Pulmonary congestion is typically not seen because equalization of diastolic pressures constrains the pulmonary capillary wedge pressure to the intra-pericardial pressure (and all other diastolic pressures).
Causes
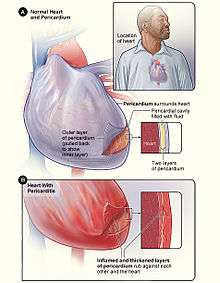
Figure B shows the heart with pericarditis. The inset image is an enlarged cross-section that shows the inflamed and thickened layers of the pericardium.[11]
Infectious
Pericarditis may be caused by viral, bacterial, or fungal infection.
In the developed world viruses are believed to be the cause of about 85% of cases.[5] In the developing world tuberculosis is a common cause but it is rare in the developed world.[5]
Viral causes include coxsackievirus, herpesvirus, mumps virus, and HIV among others.[3]
Pneumococcus or tuberculous pericarditis are the most common bacterial forms. Anaerobic bacteria can also be a rare cause.[12] Fungal pericarditis is usually due to histoplasmosis, or in immunocompromised hosts Aspergillus, Candida, and Coccidioides. The most common cause of pericarditis worldwide is infectious pericarditis with Tuberculosis.
Other
- Idiopathic: No identifiable cause found after routine testing.[3]
- Autoimmune disease: systemic lupus erythematosus, rheumatic fever[3]
- Myocardial infarction (Dressler's syndrome)[3]
- Trauma to the heart[3]
- Uremia (uremic pericarditis)[3]
- Cancer[3]
- Side effect of some medications, e.g. isoniazid, cyclosporine, hydralazine, warfarin, and heparin
- Radiation induced[3]
- Aortic dissection[3]
- Postpericardiotomy syndrome - such as after CABG surgery[3]
Diagnosis
Laboratory tests
Laboratory values can show increased urea (BUN), or increased blood creatinine in cases of uremic pericarditis. Generally however, laboratory values are normal, but if there is a concurrent myocardial infarction (heart attack) or great stress to the heart, laboratory values may show increased cardiac markers like Troponin (I, T), CK-MB, Myoglobin, and LDH1 (Lactase Dehydrogenase isotype 1). The preferred initial diagnostic testing is the ECG which will show a 12-lead electrocardiogram with diffuse, non-specific, concave ("saddle-shaped"), ST segment-elevations all leads except aVR and V1[10] and PR segment-depression possible in any lead except aVR;[10] sinus tachycardia, and low-voltage QRS complexes can also be seen if there is subsymptomatic levels of pericardial effusion. The PR depression is often seen early in the process as the thin atria are affected more easily than the ventricles by the inflammatory process of the pericardium.
Since the mid-19th Century, retrospective diagnosis of pericarditis has been made upon the finding of adhesions of the pericardium.[13] When pericarditis is diagnosed clinically, the underlying cause is often never known; it may be discovered in only 16-22 percent of patients with acute pericarditis.
Imaging
-
Ultrasounds showing a pericardial effusion in someone with pericarditis
-
A pericardial effusion as seen on CXR in someone with pericarditis
Classification
Pericarditis can be classified according to the composition of the fluid that accumulates around the heart.[14]
Types of pericarditis include the following:
Acute vs. chronic
Depending on the time of presentation and duration, pericarditis is divided into "acute" and "chronic" forms. Acute pericarditis is more common than chronic pericarditis, and can occur as a complication of infections, immunologic conditions, or even as a result of a heart attack (myocardial infarction). Chronic pericarditis however is less common, a form of which is constrictive pericarditis. The following is the clinical classification of acute vs. chronic:
- Clinically: Acute (<6 weeks), Subacute (6 weeks to 6 months) and Chronic (>6 months)
Treatment
The treatment in viral or idiopathic pericarditis is with aspirin,[10] or non-steroidal anti-inflammatory drugs (NSAIDs such as ibuprofen).[3] Colchicine may be added to the above as it decreases the risk of further episodes of pericarditis.[3][15]
Severe cases may require one or more of the following:
- pericardiocentesis to treat pericardial effusion/tamponade
- antibiotics to treat tuberculosis or other bacterial causes.
- steroids are used in acute pericarditis but are not favored because they increase the chance of recurrent pericarditis.
- in rare cases, surgery
- in cases of constrictive pericarditis, pericardiectomy
Epidemiology
About 30% of people with viral pericarditis or pericarditis of an unknown cause have one or several recurrent episodes.[16]
References
- 1 2 3 "What Is Pericarditis?". NHLBI. September 26, 2012.
- 1 2 3 "What Are the Signs and Symptoms of Pericarditis?". NHLBI. September 26, 2012. Retrieved 28 September 2016.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Tingle, LE; Molina, D; Calvert, CW (15 November 2007). "Acute pericarditis.". American family physician. 76 (10): 1509–14. PMID 18052017.
- ↑ "What Causes Pericarditis?". NHLBI. September 26, 2012. Retrieved 28 September 2016.
- 1 2 3 4 Imazio, M; Gaita, F; LeWinter, M (13 October 2015). "Evaluation and Treatment of Pericarditis: A Systematic Review.". JAMA. 314 (14): 1498–506. doi:10.1001/jama.2015.12763. PMID 26461998.
- ↑ "How Is Pericarditis Treated?". NHLBI. September 26, 2012. Retrieved 28 September 2016.
- 1 2 Imazio, M; Gaita, F (July 2015). "Diagnosis and treatment of pericarditis.". Heart (British Cardiac Society). 101 (14): 1159–68. PMID 25855795.
- ↑ McConaghy, JR; Oza, RS (1 February 2013). "Outpatient diagnosis of acute chest pain in adults.". American family physician. 87 (3): 177–82. PMID 23418761.
- ↑ "Who Is at Risk for Pericarditis?". NHLBI. September 26, 2012. Retrieved 28 September 2016.
- 1 2 3 4 5 6 American College of Physicians (ACP). "Pericardial disease". Medical Knowledge Self-Assessment Program (MKSAP-15): Cardiovascular Medicine. p. 64. ISBN 9781934465288.
- ↑ "Pericarditis". nhlbi.nih.gov. Retrieved 5 August 2014.
- ↑ Brook I (2009). "Pericarditis caused by anaerobic bacteria". Int J Antimicrob Agents: 297–300.
- ↑ Austin Flint (1862). "Lectures on the diagnosis of diseases of the heart: Lecture VIII". American Medical Times: Being a weekly series of the New York Journal of Medicine. 5 (July to December): 309–311.
- ↑ images
- ↑ Alabed, S; Cabello, JB; Irving, GJ; Qintar, M; Burls, A (Aug 28, 2014). "Colchicine for pericarditis.". The Cochrane database of systematic reviews. 8: CD010652. doi:10.1002/14651858.CD010652.pub2. PMID 25164988.
- ↑ Imazio, M; Gaita, F; LeWinter, M (13 October 2015). "Evaluation and Treatment of Pericarditis: A Systematic Review.". JAMA. 314 (14): 1498–506. doi:10.1001/jama.2015.12763. PMID 26461998.
External links
- Pericarditis — Cleveland Clinic
- Pericarditis — National Library of Medicine
- Pericarditis — National Heart Lung Blood Institute
- Troughton RW, Asher CR, Klein AL (February 2004). "Pericarditis". Lancet. 363 (9410): 717–27. doi:10.1016/S0140-6736(04)15648-1. PMID 15001332.
- Maisch B, Seferović PM, Ristić AD, et al. (April 2004). "Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology". Eur. Heart J. 25 (7): 587–610. doi:10.1016/j.ehj.2004.02.002. PMID 15120056.