Antigen presentation
Antigen presentation describes a vital immune process. Immune cells cannot penetrate other cells, which may be infected with viruses or bacteria, and thus rely on information conveyed by fragments of intracellular components being presented on major histocompatibility complex (MHC) molecules on the cell surface. Likewise, many pathogens are too large to be recognised directly by immune cells, and must first be digested into smaller fragments that can be presented by specialised antigen-presenting cells (APCs), such as dendritic cells and macrophages.
Intracellular antigens: Class I
Because body cells often become infected, cytotoxic T cells regularly patrol these, and whenever they encounter signs of disease, they initiate processes to destroy the potentially harmful cell. Some cases will involve ingested microbes, or the cell being inundated with viral matter. To effect recognition, all nucleated cells in the body (along with platelets) display class I major histocompatibility complex or MHC molecules on their surface; these present peptides, or protein fragments, sourced from within the cell. If the cell is healthy, only “self” peptides derived from the cell itself will be displayed; if however it has been hijacked by microbes “non-self” or foreign peptides will appear alongside them. Cytotoxic T cells can then monitor these MHC molecules, and easily recognise dangerous cells. In the presentation process the host cell breaks its own cytoplasmic proteins down into small peptides with an enzymatic complex, the proteasome. The carrier protein TAP, the transporter associated with antigen processing, then transports the peptides into the endoplasmic reticulum, where it is coupled to an MHC molecule and transported to the cell surface.
In the endoplasmic reticulum, the peptide is anchored to the peptide-binding groove on the floor of the α1-α2 heterodimer of the MHC class I molecule.
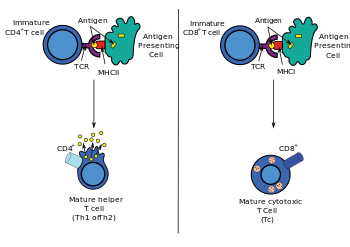
CD8+ Cytotoxic T cells are programmed to recognise peptides coupled to the MHC Class I molecules on all nucleated cells. Cytotoxic T cells (also known as TC, killer T cell, or cytotoxic T-lymphocyte (CTL)) are a population of T cells that are specialized for inducing the death of other cells. Recognition of antigenic peptides through Class I by CTLs leads to the killing of the target cell, which may be infected by virus, intracytoplasmic bacterium, or are otherwise damaged or dysfunctional. On the other hand, tolerated peptides from physiological protein turnover in healthy cells will be ignored. By inducing cytotoxicity in the diseased cells, cytotoxic T cells ensure the body remains healthy; the eliminated cells can be replaced by healthy cells.
Extracellular antigens: Class II
Dendritic cells (DCs) phagocytose exogenous pathogens such as bacteria, parasites, and toxins in the tissues and then migrate, via chemotactic signals, to T cell-enriched lymph nodes. During migration, DCs undergo a process of maturation in which they lose phagocytic capacity and develop an increased ability to communicate with T-cells in the lymph nodes. This maturation process is dependent on signaling from other pathogen-associated molecular pattern (PAMP) molecules through pattern recognition receptors, such as the members of the Toll-like receptor family.
The DC uses lysosome-associated enzymes to digest pathogen-associated proteins into smaller peptides. In the lymph node, the DC will display these antigenic peptides on its surface by coupling them to MHC Class II molecules. This MHC:antigen complex is then recognized by T cells passing through the lymph node. Exogenous antigens are usually displayed on MHC Class II molecules, which interact with CD4+ helper T cells. CD4+ lymphocytes, or TH, are immune response mediators, and play an important role in establishing and maximizing the capabilities of the adaptive immune response.
Expression of Class II is more restricted than Class I. High levels of Class II are found on dendritic cells, but can also be observed on activated macrophages, B cells, and several other host cell types in inflammatory conditions.
Intact antigens: Presentation to B cells
B-cell receptors bind to intact, undigested antigens, rather than to proteins which have been digested in lysosomes and presented by an MHC molecules. Small antigens sometimes encounter B cells after diffusing on their own to lymph nodes, but larger pieces of intact antigen appear to be presented to B cells by follicular dendritic cells and macrophages. It appears that the macrophages which present to B cells express comparatively low levels of lysosomal enzymes and thus are less likely to digest the antigen they have captured before presenting it.[1][2]
See also
References
- ↑ Batista, Facundo D.; Harwood, Naomi E. (January 2009). "The who, how and where of antigen presentation to B cells". Nature Reviews Immunology. Macmillan Publishers Limited. 9: 15–27. doi:10.1038/nri2454. Retrieved 25 May 2016.
- ↑ Harwood, Naomi E; Batista, Facundo D (Dec 17, 2010). "Antigen presentation to B cells". F1000 Biol Reports. Faculty of 1000 Ltd. 2: 87. doi:10.3410/B2-87. PMC 3026618
 .
.
External links
- ImmPort - Gene summaries, ontologies, pathways, protein/protein interactions and more for genes involved in antigen processing and presentation
- antigen presentation at the US National Library of Medicine Medical Subject Headings (MeSH)