Candida glabrata
| Candida glabrata | |
|---|---|
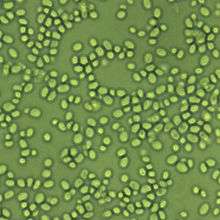 | |
| Candida glabrata 1600x | |
| Scientific classification | |
| Kingdom: | Fungi |
| Division: | Ascomycota |
| Subdivision: | Saccharomycotina |
| Class: | Saccharomycetes |
| Order: | Saccharomycetales |
| Family: | Saccharomycetaceae |
| Genus: | Candida |
| Species: | C. glabrata |
| Binomial name | |
| Candida glabrata (H.W.Anderson) S.A.Mey. & Yarrow (1978) | |
| Synonyms | |
|
Cryptococcus glabratus H.W.Anderson (1917) | |
Candida glabrata is a haploid yeast of the genus Candida, previously known as Torulopsis glabrata. This species of yeast is non-dimorphic and no mating activity has been observed. Until recently, C. glabrata was thought to be a primarily non-pathogenic organism. However, with the ever increasing population of immunocompromised individuals, trends have shown C. glabrata to be a highly opportunistic pathogen of the urogenital tract, and of the bloodstream (Candidemia). It is especially prevalent in the elderly and HIV positive people.
There are two widely cited potential virulence factors that contribute to the pathogenicity of C. glabrata. The first is a series of adhesins coded by the EPA (epithelial adhesin) genes. These genes, located in the subtelomeric region, can respond to environmental cues that allow them to be expressed en masse so the organism can adhere to biotic and abiotic surfaces in microbial mats. This is also the suspected mechanism by which C. glabrata forms microbial "biofilms" on urinary catheters, and less commonly in-dwelling IV catheters. It also causes problems with dental devices, such as dentures.[1]
Diagnosis
Cultures are an effective method for identifying non-albicans vaginal infections. Urinalyses are less accurate in this process. The culture may take several days to grow, but the identification of the yeast species is quick once the yeast is isolated. Skin disease diagnosis is difficult, as cultures collected from swabs and biopsies will test negative for fungus and a special assessment is required. Listed under the 'Rare Diseases' database on the NIH web site, Torulopsis glabrata, or Candida glabrata can also be found on the CDC's web site.[2] Although listed as the second most virulent yeast after Candida albicans, the fungus is becoming more and more resistant to common treatments like fluconazole. Like many Candida species, C. glabrata resistance to Echinocandin is also inceasing, leaving expensive and toxic antifungal treatments available for those infected.[3] Although high mortality rates are listed, assessment of the critical nature of a glabrata infection is a gray area. Another promising diagnostic tool is the T2Candida Panel, which in addition to glabrata, can also identify albicans, tropicalis, kruzei and parapsilosis direct from whole blood without requiring a blood culture. The T2 Candida Panel is manufactured by T2 Biosystems, Inc and received FDA approval in September 2014.
Treatment
A major phenotype and potential virulence factor that C. glabrata possesses is low-level intrinsic resistance to the azole drugs, which are the most commonly prescribed antifungal (antimycotic) medications. These drugs, including fluconazole and ketoconazole, are "not effective in 15-20% of cases"[4] against C. glabrata. It is still highly vulnerable to polyene drugs such as amphotericin B and nystatin, along with variable vulnerability to flucytosine and caspofungin. However intravenous amphotericin B is a drug of last resort, causing among other side effects, chronic renal failure. Amphotericin B vaginal suppositories are used as an effective form of treatment in combination with boric acid capsules as they are not absorbed into the blood stream.
A first-line treatment for vaginal infections may be the use of terconazole 7-day cream. Several courses may be needed. The cure-rate for this treatment is approximately 40%. Recurrences are common, causing chronic infections and spread to other areas such as skin and scalp. Blood infections might well be best assessed per symptoms if other areas are involved.
An experimental, but effective second-line treatment for chronic infections, is the use of boric acid. Compounding pharmacies can create boric acid vaginal suppositories. Use of Vitamin E oil may be used in conjunction to combat irritation. Amphotericin B vaginal suppositories have also been used in case studies to treat chronic infections, both symptomatic and asymptomatic. Borax and boric acid may be used for persistent scalp and skin infections.
References
- ↑ Bethea, E. K.; Carver, B. J.; Montedonico, A. E.; Reynolds, T. B. (2009). "The inositol regulon controls viability in Candida glabrata". Microbiology. 156 (2): 452–462. doi:10.1099/mic.0.030072-0.
- ↑ http://www.cdc.gov/fungal/antifungal-resistance.html
- ↑ http://www.cdc.gov/fungal/antifungal-resistance.html
- ↑ Fidel F, Vazquez J, Sobel J (1999). "Candida glabrata: Review of Epidemiology, Pathogenesis, and Clinical Disease with Comparison to C. albicans". Clinical Microbiology Reviews. 12 (1): 80–96. PMC 88907
 . PMID 9880475.
. PMID 9880475.
External links
- Dr. Fungus's "Candida inconspicua"
- Genolevures: Candida glabrata, Genome
- Candida glabrata genome map