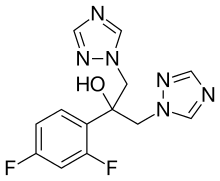
Fluconazole
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Diflucan, Celozole |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a690002 |
| License data |
|
| Pregnancy category | |
| Routes of administration | Oral, IV, topical |
| ATC code | D01AC15 (WHO) J02AC01 (WHO) |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | >90% (oral) |
| Protein binding | 11–12% |
| Metabolism | Hepatic 11% |
| Biological half-life | 30 hours (range 20-50 hours) |
| Excretion | Renal 61-88% |
| Identifiers | |
| |
| CAS Number |
86386-73-4 |
| PubChem (CID) | 3365 |
| DrugBank |
DB00196 |
| ChemSpider |
3248 |
| UNII |
8VZV102JFY |
| KEGG |
D00322 |
| ChEBI |
CHEBI:46081 |
| ChEMBL |
CHEMBL106 |
| Chemical and physical data | |
| Formula | C13H12F2N6O |
| Molar mass | 306.271 g/mol |
| 3D model (Jmol) | Interactive image |
| |
| |
| (verify) | |
Fluconazole is an antifungal medication that is given either by mouth or intravenously. It is used to treat a variety of fungal infections, especially Candida infections of the vagina (yeast infections), mouth, throat, and bloodstream. It is also used to prevent infections in people with weak immune systems, including those with neutropenia due to cancer chemotherapy, transplant patients, and premature babies.
In those who are pregnant it may increase the risk of miscarriage.[1]
Fluconazole was developed by scientists at Pfizer and was first marketed in 1990. It is now available as an inexpensive generic drug. It is on the World Health Organization's List of Essential Medicines, the most important medications needed in a basic health system.[2]
Medical Uses
Fluconazole is a first-generation triazole antifungal medication. It differs from earlier azole antifungals (such as ketoconazole) in that its structure contains a triazole ring instead of an imidazole ring. While the imidazole antifungals are mainly used topically, fluconazole and certain other triazole antifungals are preferred when systemic treatment is required because of their improved safety and predictable absorption when administered orally.[3]
Fluconazole's spectrum of activity includes most Candida species (but not Candida krusei or Candida glabrata), Cryptococcus neoformans, some dimorphic fungi, and dermatophytes, among others. Common uses include:[3][4][5][6][7]
- The treatment of non-systemic Candida infections of the vagina ("yeast infections"), throat, and mouth.
- Certain systemic Candida infections in people with healthy immune systems, including infections of the bloodstream, kidney, or joints. Other antifungals are usually preferred when the infection is in the heart or central nervous system, and for the treatment of active infections in people with weak immune systems.
- The prevention of Candida infections in people with weak immune systems, such as those neutropenic due to cancer chemotherapy, those with advanced HIV infections, transplant patients, and premature infants.
- As a second-line agent for the treatment of cryptococcal meningoencephalitis, a fungal infection of the central nervous system.
Resistance
Fungal resistance to drugs in the azole class tends to occur gradually over the course of prolonged drug therapy, resulting in clinical failure in immunocompromised patients (e.g., patients with advanced HIV receiving treatment for thrush or esophageal Candida infection).[8]
In C. albicans, resistance occurs by way of mutations in the ERG11 gene, which codes for 14α-demethylase. These mutations prevent the azole drug from binding, while still allowing binding of the enzyme's natural substrate, lanosterol. Development of resistance to one azole in this way will confer resistance to all drugs in the class. Another resistance mechanism employed by both C. albicans and C. glabrata is increasing the rate of efflux of the azole drug from the cell, by both ATP-binding cassette and major facilitator superfamily transporters. Other gene mutations are also known to contribute to development of resistance.[8] C. glabrata develops resistance by up regulating CDR genes, and resistance in C. krusei is mediated by reduced sensitivity of the target enzyme to inhibition by the agent.[9]
The full spectrum of fungal susceptibility and resistance to fluconazole can be found in the TOKU-E's product data sheet.[10] According to the United States Centers for Disease Control, fluconzole resistance among Candida strains in the U.S. is about 7%.[11]
Contraindications
Fluconazole is contraindicated in patients who:[7]
- Have known hypersensitivity to other azole medicines such as ketoconazole
- Are taking terfenadine, if 400 mg per day multidose of fluconazole is administered
- Concomitant administration of fluconazole and quinidine, especially when fluconazole is administered in high dosages
- Take SSRIs such as fluoxetine or sertraline
Adverse effects
Adverse drug reactions associated with fluconazole therapy include:[7]
- Common (≥1% of patients): rash, headache, dizziness, nausea, vomiting, abdominal pain, diarrhea, and/or elevated liver enzymes
- Infrequent (0.1–1% of patients): anorexia, fatigue, constipation
- Rare (<0.1% of patients): oliguria, hypokalaemia, paraesthesia, seizures, alopecia, Stevens–Johnson syndrome, thrombocytopenia, other blood dyscrasias, serious hepatotoxicity including liver failure, anaphylactic/anaphylactoid reactions
- Very rare: prolonged QT interval, torsades de pointes
- FDA is now saying treatment with chronic, high doses of fluconazole during the first trimester of pregnancy may be associated with a rare and distinct set of birth defects in infants.[12]
If taken during pregnancy it may result in harm.[13][14] These cases of harm; however, were only in women who took large doses for most of the first trimester.[13] It is of the triazole class.
Fluconazole is secreted in human milk at concentrations similar to plasma. Therefore, the use of fluconazole in lactating mothers is not recommended.[15]
Fluconazole therapy has been associated with QT interval prolongation, which may lead to serious cardiac arrhythmias. Thus, it is used with caution in patients with risk factors for prolonged QT interval, such as electrolyte imbalance or use of other drugs that may prolong the QT interval (particularly cisapride and pimozide).
Fluconazole has also rarely been associated with severe or lethal hepatotoxicity, so liver function tests are usually performed regularly during prolonged fluconazole therapy. In addition, it is used with caution in patients with pre-existing liver disease.[16]
Some people are allergic to azoles, so those allergic to other azole drugs might be allergic to fluconazole.[17] That is, some azole drugs have adverse side-effects. Some azole drugs may disrupt estrogen production in pregnancy, affecting pregnancy outcome. [18]
Fluconazole taken at low doses is in FDA pregnancy category C. However, high doses have been associated with a rare and distinct set of birth defects in infants. If taken at these doses, the pregnancy category is changed from category C to category D. Pregnancy category D means there is positive evidence of human fetal risk based on human data. In some cases, the potential benefits from use of the drug in pregnant women with serious or life-threatening conditions may be acceptable despite its risks. Fluconazole should not be taken during pregnancy or if one could become pregnant during treatment without first consulting a doctor.[19] Oral fluconazole is not associated with a significantly increased risk of birth defects overall, although it does increase the odds ratio of tetralogy of Fallot, but the absolute risk is still low.[20] Women using flucanozol during pregnancy have a 50% higher risk of spontaneous abortion.[21]
Fluconazole should not be taken with cisapride (Propulsid) due to the possibility of serious, even fatal, heart problems. In rare cases, severe allergic reactions including anaphylaxis may occur.
Powder for oral suspension contains sucrose and should not be used in patients with hereditary fructose, glucose/galactose malabsorption or sucrase-isomaltase deficiency. Capsules contain lactose and should not be given to patients with rare hereditary problems of galactose intolerance, Lapp lactase deficiency, or glucose-galactose malabsorption [22]
Drug interactions
Fluconazole is an inhibitor of the human cytochrome P450 system, particularly the isozyme CYP2C19 (CYP3A4 and CYP2C9 to lesser extent) [23] In theory, therefore, fluconazole decreases the metabolism and increases the concentration of any drug metabolised by these enzymes. In addition, its potential effect on QT interval increases the risk of cardiac arrhythmia if used concurrently with other drugs that prolong the QT interval. Berberine has been shown to exert synergistic effects with fluconazole even in drug-resistant Candida albicans infections.[24] Fluconazole may decrease the metabolism of benzodiazepines. Fluconazole may increase the serum concentration of Citalopram (Risk X: avoid combination). Fluconazole may increase the serum concentration of Erythromycin (Risk X: avoid combination).[23]
Mechanism of action
Like other imidazole- and triazole-class antifungals, fluconazole inhibits the fungal cytochrome P450 enzyme 14α-demethylase. Mammalian demethylase activity is much less sensitive to fluconazole than fungal demethylase. This inhibition prevents the conversion of lanosterol to ergosterol, an essential component of the fungal cytoplasmic membrane, and subsequent accumulation of 14α-methyl sterols.[16] Fluconazole is primarily fungistatic; however, it may be fungicidal against certain organisms in a dose-dependent manner, specifically Cryptococcus.[25]
It is interesting to note, when fluconazole was in development at Pfizer, it was decided early in the process to avoid producing any chiral centers in the drug so subsequent synthesis and purification would not encounter difficulties with enantiomer separation and associated variations in biological effect. A number of related compounds were found to be extremely potent teratogens, and were subsequently discarded.
Pharmacokinetics
Following oral dosing, fluconazole is almost completely absorbed within two hours. Bioavailability is not significantly affected by the absence of stomach acid. Concentrations measured in the urine, tears, and skin are approximately 10 times the plasma concentration, whereas saliva, sputum, and vaginal fluid concentrations are approximately equal to the plasma concentration, following a standard dose range of between 100 mg and 400 mg per day. The elimination half-life of fluconazole follows zero order kinetics, and only 10% of elimination is due to metabolism, the remainder being excreted in urine and sweat. Patients with impaired renal function will be at risk of overdose.
In a bulk powder form, it appears as a white crystalline powder, and it is very slightly soluble in water and soluble in alcohol.[26]
Brands
Fluconazole is sold as a single 150 mg dose over the counter in Canada under the brand names Monicure / Monistat and Canesten.[27] In Mexico, it is sold over the counter as Alfumet, Afungil or Dofil. It is marketed under the brand name Candivast in the Persian Gulf area. In Colombia, it is marketed as Batén by Laboratorios Bussié. In Panama, it is marketed under the name Ibarin from different manufacturers. In Egypt, it is marketed under the names Diflucan, Flucoral, Fungican, Triconal. The No.1 brand in India is Zocon, available as Tablets, Lotion, Dusting Powder, Transgel and Eye Drop.
See also
References
- ↑ "Fluconazole (Diflucan): Drug Safety Communication - FDA Evaluating Study Examining Use of Oral Fluconazole (Diflucan) in Pregnancy". FDA. 2016-04-26. Retrieved 29 April 2016.
- ↑ "WHO Model List of EssentialMedicines" (PDF). World Health Organization. October 2013. Retrieved 22 April 2014.
- 1 2 "US Pharmacist". Retrieved 2015-01-28.
- ↑ "US Prescribing Information" (PDF). Retrieved 2015-01-28.
- ↑ "IDSA Guidelines: Candida Infections" (PDF). Retrieved 2015-01-28.
- ↑ "IDSA Guidelines: Cryptococcal Infections" (PDF). Retrieved 2015-01-28.
- 1 2 3 Rossi S, editor. Australian Medicines Handbook 2006. Adelaide: Australian Medicines Handbook; 2006. ISBN 0-9757919-2-3
- 1 2 Bennett J. E. (2011). "57. Antifungal Agents". In L.L. Brunton; B.A. Chabner; B.C. Knollmann. Goodman & Gilman's The Pharmacological Basis of Therapeutics, 12e. Retrieved May 22, 2012.
- ↑ http://labeling.pfizer.com/ShowLabeling.aspx?id=575
- ↑ Spectrum of fungal susptibility and resistance to fluconazole
- ↑ "Antifungal Resistance | Fungal Disease | CDC".
- ↑ http://www.drugs.com/fda/diflucan-fluconazole-safety-communication-long-term-during-pregnancy-may-associated-birth-defects-13013.html
- 1 2 "Fluconazole". Monograph. The American Society of Health-System Pharmacists. Retrieved 2014-09-27.
- ↑ "Prescribing medicines in pregnancy database". Australian Government. 3 March 2014. Retrieved 22 April 2014.
- ↑ Product information from Pfizer Inc
- 1 2 Pfizer Australia Pty Ltd. Diflucan (Australian Approved Product Information). West Ryde (NSW): Pfizer Australia; 2004.
- ↑ http://aac.asm.org/cgi/reprint/AAC.01500-08v1.pdf
- ↑ Kragie, Laura; Turner, Stephanie D.; Patten, Christopher J.; Crespi, Charles L.; Stresser, David M. (2002). "Assessing Pregnancy Risks of Azole Antifungals Using a High Throughput Aromatase Inhibition Assay". Endocrine Research. 28 (3): 129–40. doi:10.1081/ERC-120015045. PMID 12489563.
- ↑ Fluconazole, PubMed Health
- ↑ Mølgaard-Nielsen, D.; Pasternak, B. R.; Hviid, A. (2013). "Use of Oral Fluconazole during Pregnancy and the Risk of Birth Defects". New England Journal of Medicine. 369 (9): 830–839. doi:10.1056/NEJMoa1301066. PMID 23984730.
- ↑ Mølgaard-Nielsen D, Svanström H, Melbye M, Hviid A, Pasternak B (2016-01-05). "Association between use of oral fluconazole during pregnancy and risk of spontaneous abortion and stillbirth.". JAMA. 315 (1): 58–67. doi:10.1001/jama.2015.17844. ISSN 1538-3598. PMID 26746458.
- ↑ http://reference.medscape.com/drug/diflucan-fluconazole-342587#5
- 1 2 http://online.lexi.com.proxy1.lib.tju.edu/lco/action/doc/retrieve/docid/patch_f/6918
- ↑ Xu, Yi; Wang, Yan; Yan, Lan; Liang, Rong-Mei; Dai, Bao-Di; Tang, Ren-Jie; Gao, Ping-Hui; Jiang, Yuan-Ying (2009). "Proteomic Analysis Reveals a Synergistic Mechanism of Fluconazole and Berberine against Fluconazole-ResistantCandida albicans: Endogenous ROS Augmentation". Journal of Proteome Research. 8 (11): 5296–5304. doi:10.1021/pr9005074. ISSN 1535-3893. PMID 19754040. Free Full Text
- ↑ Longley, Nicky; Muzoora, Conrad; Taseera, Kabanda; Mwesigye, James; Rwebembera, Joselyne; Chakera, Ali; Wall, Emma; Andia, Irene; Jaffar, Shabbar; Harrison, Thomas S. (2008). "Dose Response Effect of High‐Dose Fluconazole for HIV‐Associated Cryptococcal Meningitis in Southwestern Uganda". Clinical Infectious Diseases. 47 (12): 1556–1561. doi:10.1086/593194. ISSN 1058-4838. PMID 18990067.
- ↑ MP Biomedicals
- ↑ Insight Pharmaceuticals. Our Products: Monicure. N.p.: Insight Pharmaceuticals, n.d.Monistat. Insight Pharmaceuticals, 2013. Web. 24 July 2013. <http://www.monistat.ca/monicure>.