Colistin
 | |
| Clinical data | |
|---|---|
| Trade names | Coly-mycinm; Coly-monas (India) |
| Pregnancy category |
|
| Routes of administration | topical, oral, intravenous, inhaled |
| ATC code | A07AA10 (WHO) J01XB01 (WHO) QJ51XB01 (WHO) |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 0% |
| Biological half-life | 5 hours |
| Identifiers | |
| |
| CAS Number |
1066-17-7 |
| PubChem (CID) | 5311054 |
| DrugBank |
DB00803 |
| ChemSpider |
4470591 |
| UNII |
Z67X93HJG1 |
| KEGG |
D02138 |
| ChEMBL |
CHEMBL501505 |
| ECHA InfoCard | 100.013.668 |
| Chemical and physical data | |
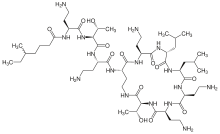
| Formula | C52H98N16O13 |
| Molar mass | 1155.4495 g/mol |
| 3D model (Jmol) | Interactive image |
| |
| |
| | |
Colistin, also known as polymyxin E, is an antibiotic produced by certain strains of the bacteria Paenibacillus polymyxa. Colistin is a mixture of the cyclic polypeptides colistin A and B and belongs to the class of polypeptide antibiotics known as polymyxins. Colistin is effective against most Gram-negative bacilli.
Colistin is a decades-old drug that fell out of favor due to its nephrotoxicity. It remains one of the last-resort antibiotics for multidrug-resistant Pseudomonas aeruginosa, Klebsiella pneumoniae, and Acinetobacter.[1] NDM-1 metallo-β-lactamase multidrug-resistant Enterobacteriaceae have also shown susceptibility to colistin.[2]
Resistance to colistin is rare. The first colistin-resistance gene that is carried in a plasmid and can be transferred between bacterial strains was described in 2016.[3] This plasmid-borne mcr-1 gene has since been isolated in China,[3] Europe[4] and the United States.[5]
History
Colistin was first isolated in Japan in 1949 from a flask of fermenting Bacillus polymyxa var. colistinus by the Japanese scientist Koyama[6] and became available for clinical use in 1959[7]
Colistimethate sodium, a less toxic prodrug, became available for injection in 1959. In the 1980's, polymyxin use was widely discontinued because of nephro- and neurotoxicity. As multi-drug resistant bacteria became more prevalent in the 1990's, colistin started to get a second look as an emergency solution, in spite of toxic effects.[8]
Administration and dosage
Forms
Two forms of colistin are available commercially: colistin sulfate and colistimethate sodium (colistin methanesulfonate sodium, colistin sulfomethate sodium). Colistin sulfate is cationic; colistimethate sodium is anionic. Colistin sulfate is stable, but colistimethate sodium is readily hydrolysed to a variety of methanesulfonated derivatives. Colistin sulfate and colistimethate sodium are eliminated from the body by different routes. With respect to Pseudomonas aeruginosa, colistimethate is the inactive prodrug of colistin. The two drugs are not interchangeable .
- Colistimethate sodium may be used to treat Pseudomonas aeruginosa infections in cystic fibrosis patients, and it has come into recent use for treating multidrug-resistant Acinetobacter infection, although resistant forms have been reported.[9][10] Colistimethate sodium has also been given intrathecally and intraventricularly in Acinetobacter baumannii and Pseudomonas aeruginosa meningitis/ventriculitis[11][12][13][14] Some studies have indicated that colistin may be useful for treating infections caused by carbapenem-resistant isolates of Acinetobacter baumannii.[10]
- Colistin sulfate may be used to treat intestinal infections, or to suppress colonic flora. Colistin sulfate is also used as topical creams, powders, and otic solutions.
- Colistin A (polymyxin E1) and colistin B (polymyxin E2) can be purified individually to research and study their effects and potencies as separate compounds.
Dosage
Colistin sulfate and colistimethate sodium may both be given intravenously, but the dosing is complicated. The very different labeling of the parenteral products of colistin methanesulfonate in different parts of the world was first revealed by Li et al.[15] Colistimethate sodium manufactured by Xellia (Colomycin injection) is prescribed in international units, but colistimethate sodium manufactured by Parkdale Pharmaceuticals (Coly-Mycin M Parenteral) is prescribed in milligrams of colistin base:
- Colomycin 1,000,000 units is 80 mg colistimethate;[16]
- Coly-mycin M 150 mg "colistin base" is 360 mg colistimethate or 4,500,000 units.[17]
Because colistin was introduced into clinical practice over 50 years ago, it was never subject to the regulations that modern drugs are subject to, and therefore there is no standardised dosing of colistin and no detailed trials on pharmacology or pharmacokinetics: The optimal dosing of colistin for most infections is therefore unknown. Colomycin has a recommended intravenous dose of 1 to 2 million units three times daily for patients weighing 60 kg or more with normal renal function. Coly-Mycin has a recommended dose of 2.5 to 5 mg/kg colistin base a day, which is equivalent to 6 to 12 mg/kg colistimethate sodium per day. For a 60 kg man, therefore, the recommended dose for Colomycin is 240 to 480 mg of colistimethate sodium, yet the recommended dose for Coly-Mycin is 360 to 720 mg of colistimethate sodium. Likewise, the recommended "maximum" dose for each preparation is different (480 mg for Colomycin and 720 mg for Coly-Mycin). Each country has different generic preparations of colistin, and the recommended dose depends on the manufacturer. This complete absence of any regulation or standardisation of dose makes intravenous colistin dosing difficult for any physician.
Colistin has been used in combination with rifampicin, and evidence of in-vitro synergy exists,[18][19] and the combination has been used successfully in patients.[20] There is also in-vitro evidence of synergy for colistimethate sodium used in combination with other antipseudomonal antibiotics.[21]
Colistimethate sodium aerosol (Promixin; Colomycin Injection) is used to treat pulmonary infections, especially in cystic fibrosis. In the UK, the recommended adult dose is 1–2 million units (80–160 mg) nebulised colistimethate twice daily.[22][23]
Mechanism of action
Colistin is a polycationic peptide and has both hydrophilic and lipophilic moieties. These cationic regions interact with the bacterial outer membrane, by displacing magnesium and calcium bacterial counter ions in the lipopolysaccharide. Hydrophobic/hydrophilic regions interact with the cytoplasmic membrane just like a detergent, solubilizing the membrane in an aqueous environment. This effect is bactericidal even in an isosmolar environment.
Spectrum of bacterial susceptibility
Colistin has been effective in treating infections caused by Pseudomonas, Escherichia, and Klebsiella species. The following represents MIC susceptibility data for a few medically significant microorganisms.
- Escherichia coli: 0.12–128 μg/ml
- Klebsiella pneumoniae: 0.25–128 μg/ml
- Pseudomonas aeruginosa: ≤0.06–16 μg/ml
Colistin in combination with other drugs are used to attack P. aeruginosa biofilm infection in lungs of CF patients.[26] Biofilms have a low oxygen environment below the surface where bacteria are metabolically inactive and colistin is highly effective in this environment. However, P. aeruginosa reside in the top layers of the biofilm, where they remain metabolically active.[27] This is because surviving tolerant cells migrate to the top of the biofilm via pili motility and form new aggregates via quorum sensing.[28] Consequently, a drug combination attacking both the inactive and active forms of P. aeruginosa is highly effective.
Resistance
Resistance to colistin is currently rare, but is described. At present, no agreement exists about how to look for colistin resistance. The fr:Société Française de Microbiologie uses a cut-off of 2 mg/l, whereas the British Society for Antimicrobial Chemotherapy sets a cutoff of 4 mg/l or less as sensitive, and 8 mg/ml or more as resistant. No standards for measuring colistin sensitivity are given in the US. The plasmid-borne mcr-1 gene has been found to confer resistance to colistin.[3]
India reported the first clear and detailed colistin-resistance study which mapped 13 colistin-resistant cases recorded over 18 months. It concluded that pan-drug resistant infections, particularly those in the blood stream, have a higher mortality. Multiple other cases were reported from other Indian hospitals.[29][30] Although resistance to polymyxins is generally less than 10%, it is higher in the Mediterranean and South-East Asia (Korea and Singapore), where colistin resistance rates are continually increasing.[31] Colistin-resistant E. coli was identified in the United States in May 2016.[32]
Use of colistin to treat Acinetobacter baumannii infections has, as with other antibiotics, led to the development of resistant bacterial strains. These resistant strains have also been shown to develop resistance to antimicrobial compounds, including LL-37 and lysozyme, produced as part of the human host's immune system.[33]
Exceptional (inherently colistin-resistant) Gram-negative bacteria
- Brucella
- Burkholderia cepacia
- Chryseobacterium indologenes
- Edwardsiella
- Elizabethkingia meningoseptica
- Francisella tularensis spp.
- Gram-negative cocci
- Helicobacter pylori
- Moraxella catarrhalis
- Morganella spp.
- Neisseria gonorrheae and Neisseria meningitidis
- Proteus
- Providencia
- Serratia
- Some strains of Stenotrophomonas maltophilia[34]
Gram-negative organisms with variable resistance to colistin
Pharmacokinetics
No clinically useful absorption of colistin occurs in the gastrointestinal tract. For systemic infection, colistin must, therefore, be given by injection. Colistimethate is eliminated by the kidneys, but colistin is supposed to be eliminated by non-renal mechanism(s) that are as yet not characterised.[35][36]
Adverse reactions
The main toxicities described with intravenous treatment are nephrotoxicity (damage to the kidneys) and neurotoxicity (damage to the nerves),[37][38][39][40] but this may reflect the very high doses given, which are much higher than the doses currently recommended by any manufacturer and for which no adjustment was made for renal disease. Neuro- and nephrotoxic effects appear to be transient and subside on discontinuation of therapy or reduction in dose.[41]
At a dose of 160 mg colistimethate IV every eight hours, very little nephrotoxicity is seen.[42][43] Indeed, colistin appears to have less toxicity than the aminoglycosides that subsequently replaced it, and it has been used for extended periods up to six months with no ill effects.[44]
The main toxicity described with aerosolised treatment is bronchospasm,[45] which can be treated or prevented with the use of beta2-agonists such as salbutamol[46] or following a desensitisation protocol.[47]
References
- ↑ Falagas ME, Grammatikos AP, Michalopoulos A (October 2008). "Potential of old-generation antibiotics to address current need for new antibiotics". Expert review of anti-infective therapy. 6 (5): 593–600. doi:10.1586/14787210.6.5.593. PMID 18847400.
- ↑ Kumarasamy KK, Toleman MA, Walsh TR, Bagaria J, Butt F, Balakrishnan R, Chaudhary U, Doumith M, Giske CG, Irfan S, Krishnan P, Kumar AV, Maharjan S, Mushtaq S, Noorie T, Paterson DL, Pearson A, Perry C, Pike R, Rao B, Ray U, Sarma JB, Sharma M, Sheridan E, Thirunarayan MA, Turton J, Upadhyay S, Warner M, Welfare W, Livermore DM, Woodford N (2010). "Emergence of a new antibiotic resistance mechanism in India, Pakistan, and the UK: a molecular, biological, and epidemiological study". The Lancet Infectious Diseases. 10 (9): 597–602. doi:10.1016/S1473-3099(10)70143-2. PMC 2933358
 . PMID 20705517.
. PMID 20705517. - 1 2 3 Lui YY, et al. (February 2016). "Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China: a microbiological and molecular biological study". The Lancet Infectious Diseases. doi:10.1016/S1473-3099(15)00424-7. Retrieved 2015-11-19.
- ↑ Maryn McKenna. "Apocalypse Pig Redux: Last-Resort Resistance in Europe". Phenomena. Retrieved 28 May 2016.
- ↑ "First discovery in United States of colistin resistance in a human E. coli infection". www.sciencedaily.com. Retrieved 2016-05-27.
- ↑ Y Koyama, A Kurosasa, A Tsuchiya, K Takakuta (1950). "A new antibiotic 'colistin' produced by spore-forming soil bacteria". J Antibiot (Tokyo). 3.
- ↑ "Colistin: An overview". www.uptodate.com. Retrieved 2016-06-06.
- ↑ Falagas M, Kasiakou S (2005). "Colistin: The Revival of Polymyxins for the Management of Multidrug-Resistant Gram-Negative Bacterial Infections". Rev Anti Infect Agen. 40.
- ↑ Reis AO, Luz DA, Tognim MC, Sader HS, Gales AC (2003). "Polymyxin-Resistant Acinetobacter spp. Isolates: What Is Next?". Emerg Infect Dis. 9: 1025–7. doi:10.3201/eid0908.030052. PMID 12971377.
- 1 2 Towner K J (2008). "Molecular Basis of Antibiotic Resistance in Acinetobacter spp.". Acinetobacter Molecular Biology. Caister Academic Press. ISBN 0-306-43902-6. [http://www.horizonpress.com/acineto.
- ↑ Benifla M, Zucker G, Cohen A, Alkan M (2004). "Successful treatment of Acinetobacter meningitis with intrathecal polymyxin". J Antimicrobial Chemotherapy. 54 (1): 290–293. doi:10.1093/jac/dkh289. PMID 15190037.
- ↑ Yagmur R, Esen F (2006). "Intrathecal colistin for treatment of Pseudomonas aeruginosa ventriculitis: report of a case with successful outcome". Critical Care. 10 (6): 428. doi:10.1186/cc5088. PMC 1794456
 . PMID 17214907.
. PMID 17214907. - ↑ Motaouakkil S, Charra B, Hachimi A, Nejmi H, Benslama A, Elmdaghri N, Belabbes H, Benbachir M (2006). "Colistin and rifampicin in the treatment of nosocomial infections from multiresistant Acinetobacter baumannii". Journal of Infection. 53 (4): 274–278. doi:10.1016/j.jinf.2005.11.019. PMID 16442632.
- ↑ Karakitsos D, Paramythiotou E, Samonis G, Karabinis A (2006). "Is intraventricular colistin an effective and safe treatment for post-surgical ventriculitis in the intensive care unit?". Acta Anaesthesiol Scand. 50 (10): 1309–1310. doi:10.1111/j.1399-6576.2006.01126.x. PMID 17067336.
- ↑ Li J, Nation RL, Turnidge JD, Milne RW, Coulthard K, Rayner CR, Paterson DL (2006). "Colistin: the re-emerging antibiotic for multidrug-resistant Gram-negative bacterial infections". Lancet Infect Dis. 6 (9): 589–601. doi:10.1016/s1473-3099(06)70580-1. PMID 16931410.
- ↑ Colomycin injection [Summary of product characteristics]. http://emc.medicines.org.uk/emc/assets/c/html/displaydoc.asp?documentid=1590
- ↑ http://www.emea.europa.eu/pdfs/vet/mrls/081502en.pdf; NB. Colistin base has an assigned potency of 30 000 IU/mg
- ↑ Ahmed N, Wahlgren NG (2003). "In vitro interaction of colistin and rifampin on multidrug-resistant Pseudomonas aeruginosa". J Chemother. 15 (4): 235–38. doi:10.1159/000069498. PMID 12686786.
- ↑ Hogg GM, Barr JG, Webb CH (1998). "In-vitro activity of the combination of colistin and rifampicin against multidrug-resistant strains of Acinetobacter baumannii". J Antimicrob Chemother. 41 (4): 494–95. doi:10.1093/jac/41.4.494.
- ↑ Petrosillo N, Chinello P, Proietti MF, Cecchini L, Masala M, Franchi C, Venditti M, Esposito S, Nicastri E (2005). "Combined colistin and rifampicin therapy for carbapenem-resistant Acinetobacter baumannii infections: clinical outcome and adverse events". Clin Microbiol Infect. 11 (8): 682–83. doi:10.1111/j.1469-0691.2005.01198.x. PMID 16008625.
- ↑ MacGowan AP, Rynn C, Wootton M, Bowker KE, Holt HA, Reeves DS (1999). "In vitro assessment of colistin's antipseudomonal antimicrobial interactions with other antibiotics". Clin Microbiol Infect. 5: 32–36. doi:10.1111/j.1469-0691.1999.tb00095.x.
- ↑ Promixin [Summary of Product Characteristics] http://emc.medicines.org.uk/emc/assets/c/html/displaydoc.asp?documentid=13532
- ↑ Colomycin Injection [Summary of Product Characteristics] http://emc.medicines.org.uk/emc/assets/c/html/displaydoc.asp?documentid=1590
- ↑ "Polymyxin E (Colistin) - The Antimicrobial Index Knowledgebase - TOKU-E". Retrieved 28 May 2016.
- ↑ http://www.toku-e.com/Assets/MIC/Colistin%20sulfate%20USP.pdf
- ↑ "Colistin-Tobramycin Combinations Are Superior to Monotherapy Concerning the Killing of Biofilm Pseudomonas aeruginosa". Retrieved 28 May 2016.
- ↑ "Tolerance to the antimicrobial peptide colistin in Pseudomonas aeruginosa biofilms is linked to metabolically active cells, and depends on the pmr and mexAB-oprM genes". Retrieved 28 May 2016.
- ↑ Chua SL, Yam JKH, Sze KS, Yang L (2016). "Selective labelling and eradication of antibiotic-tolerant bacterial populations in Pseudomonas aeruginosa biofilms". Nat Commun. 7:10750. doi:10.1038/ncomms10750. PMID 26892159.
- ↑ "New worry: Resistance to 'last antibiotic' surfaces in India". Dec 28, 2014.
- ↑ "Emergence of Pan drug resistance amongst gram negative bacteria! The First case series from India". Dec 2014.
- ↑ Bialvaei AZ, Samadi Kafil H (19 March 2015). "Colistin, mechanisms and prevalence of resistance". Curr Med Res Opin. 31 (4): 707–21. doi:10.1185/03007995.2015.1018989. PMID 25697677.
- ↑ "Discovery of first mcr-1 gene in E. coli bacteria found in a human in United States". cdc.gov. U.S. Department of Health and Human Services. 31 May 2016. Retrieved 6 July 2016.
- ↑ Napier BA, Burd EM, Satola SW, Cagle SM, Ray SM, McGann P, Pohl J, Lesho EP, Weiss DS (21 May 2013). "Clinical Use of Colistin Induces Cross-Resistance to Host Antimicrobials in Acinetobacter baumannii". MBio. 4 (3): e00021–13–e00021–13. doi:10.1128/mBio.00021-13. PMID 23695834.
- ↑ Markou N, Apostolakos H, Koumoudiou C, Athanasiou M, Koutsoukou A, Alamanos I, Gregorakos L (2003). "Intravenous colistin in the treatment of sepsis from multiresistant Gram-negative bacilli in critically ill patients". Crit Care. 7 (5): R78–83. doi:10.1186/cc2358. PMC 270720
 . PMID 12974973.
. PMID 12974973. - ↑ Li J, Milne RW, Nation RL, Turnidge JD, Smeaton TC, Coulthard K (2004). "Pharmacokinetics of colistin methanesulphonate and colistin in rats following an intravenous dose of colistin methanesulphonate". J Antimicrob Chemother. 53 (5): 837–40. doi:10.1093/jac/dkh167. PMID 15044428.
- ↑ Li J, Milne RW, Nation RL, Turnidge JD, Smeaton TC, Coulthard K (2003). "Use of High-Performance Liquid Chromatography To Study the Pharmacokinetics of Colistin Sulfate in Rats following Intravenous Administration". Antimicrob Agents Chemother. 47 (5): 1766–70. doi:10.1128/AAC.47.5.1766-1770.2003. PMC 153303
 . PMID 12709357.
. PMID 12709357. - ↑ Wolinsky E, Hines JD (1962). "Neurotoxic and nephrotoxic effects of colistin in patients with renal disease". N Engl J Med. 266 (15): 759–68. doi:10.1056/NEJM196204122661505. PMID 14008070.
- ↑ Koch-Weser J, Sidel VW, Federman EB, Kanarek P, Finer DC, Eaton AE (1970). "Adverse effects of sodium colistimethate. Manifestations and specific reaction rates during 317 courses of therapy". Annals of Internal Medicine. 72 (6): 857–68. doi:10.7326/0003-4819-72-6-857. PMID 5448745.
- ↑ Ledson MJ, Gallagher MJ, Cowperthwaite C, Convery RP, Walshaw MJ (1998). "Four years' experience of intravenous colomycin in an adult cystic fibrosis unit". Eur Respir J. 12 (3): 592–94. doi:10.1183/09031936.98.12030592. PMID 9762785.
- ↑ Li J, Nation RL, Milne RW, Turnidge JD, Coulthard K (2005). "Evaluation of colistin as an agent against multi-resistant Gram-negative bacteria". Int J Antimicrob Agents. 25 (1): 11–25. doi:10.1016/j.ijantimicag.2004.10.001. PMID 15620821.
- ↑ Beringer P (2001). "The clinical use of colistin in patients with cystic fibrosis". Current Opinion in Pulmonary Medicine. 7 (6): 434–440. doi:10.1097/00063198-200111000-00013.
- ↑ Conway SP, Etherington C, Munday J, Goldman MH, Strong JJ, Wootton M (2000). "Safety and tolerability of bolus intravenous colistin in acute respiratory exacerbation in adults with cystic fibrosis". Annals of Pharmacotherapy. 34 (11): 1238–42. doi:10.1345/aph.19370. PMID 11098334.
- ↑ Littlewood JM, Koch C, Lambert PA, Høiby N, Elborn JS, Conway SP, Dinwiddie R, Duncan-Skingle F (2000). "A ten year review of Colomycin". Respir Med. 94 (7): 632–40. doi:10.1053/rmed.2000.0834. PMID 10926333.
- ↑ Stein A, Raoult D (2002). "Colistin: an antimicrobial for the 21st century?". Clin Infect Dis. 35 (7): 901–2. doi:10.1086/342570. PMID 12228836.
- ↑ Maddison J, Dodd M, Webb AK (1994). "Nebulized colistin causes chest tightness in adults with cystic fibrosis". Respir Med. 88 (2): 145–147. doi:10.1016/0954-6111(94)90028-0.
- ↑ Kamin W, Schwabe A, Krämer I (2006). "Inhalation solutions: which one are allowed to be mixed? Physico-chemical compatibility of drug solutions in nebulizers". J Cyst Fibros. 5 (4): 205–213. doi:10.1016/j.jcf.2006.03.007. PMID 16678502.
- ↑ Domínguez-Ortega J, Manteiga E, Abad-Schilling C, Juretzcke MA, Sánchez-Rubio J, Kindelan C (2007). "Induced tolerance to nebulized colistin after severe reaction to the drug". J Investig Allergol Clin Immunol. 17 (1): 59–61. PMID 17323867.
Further reading
Resistance
- Reardon, Sara (21 December 2015). "Spread of antibiotic-resistance gene does not spell bacterial apocalypse — yet". Trend Watch. Nature. Retrieved 22 December 2015.

External links
- Colistin topics page (bibliography) on Science.gov
- Protocol for PCR detection of the gene mcr-1 gene on the National Food Institute website at the Technical University of Denmark