Tinea barbae
| Tinea barbæ | |
|---|---|
 | |
| Tinea barbæ or "barber's itch" | |
| Classification and external resources | |
| Specialty | infectious disease |
| ICD-10 | B35.0 (ILDS B35.040) |
| ICD-9-CM | 110.0 |
| eMedicine | derm/419 |
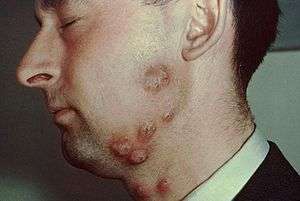
Tinea barbæ (also known as "Barber's itch,"[1] "Ringworm of the beard,"[2] and "Tinea sycosis"[1]:301) is a fungal infection of the hair. Tinea barbae is due to a dermatophytic infection around the bearded area of men. Generally, the infection occurs as a follicular inflammation, or as a cutaneous granulomatous lesion, i.e. a chronic inflammatory reaction. It is one of the causes of Folliculitis. It is most common among agricultural workers, as the transmission is more common from animal-to-human than human-to-human. The most common causes are Trichophyton mentagrophytes and T. verrucosum.
Transmission
The transmission of Tinea Barbae to humans occurs through contact of an infected animal to the skin of a human.[3] Infection can occasionally be transmitted through contact of infected animal hair on human skin. Tinea Barbae is very rarely transmitted through human to human contact but is not completely impossible.[3]
Symptoms
Main symptoms that occur when affected with Tinea Barbae is pimple or blister amongst affected area, swelling and redness around infected area, red and lumpy skin on infected area.[5] Crusting around hairs in infected area will occur, hairs on infected area will also be effortless to pull out.[5] Tinea Barbae can be itchy or painful to touch but these symptoms do not always occur.[5]
Diagnosis
Diagnosis of Tinea Barbae will firstly include questions being asked from doctors about interactions with farm animals and lifestyle experiences.[3] Doctor will then gain knowledge on possible disease by microscopy, this is viewing the skin under a microscope to get an enlarge view of infected area. Skin scraping and removal of hairs on infected area will occur for medical examination.[5] To acquire causation of Tinea Barbae putting infected area under ultraviolet light can achieve this, as infection caused by animal and human contact will not show up as fluorescent under the ultraviolet light, compared to other causes of this disease.[3]
Treatment
Treatment that will occur once Tinea Barbae is diagnosed will vary on the case of the infection, if it is a moderate case of Tinea Barbaea the individual will be given topical antifungal medications.[5] Topical antifungal medications will come in the form of cream, which can normally be obtained over the counter.[5] This process is only used during mild cases of Tinea Barbae, if there is a more serious case of Tinea Barbae the treatment used will be oral antifungal medications.[5] Oral antifungal medications come in the form of tablets and each patient will receive their individual dose of tablets depending on the severity of their infection.[5]
Prevention
To prevent catching this disease, animals should be put in an environment that causes minimal contact of animals and humans[3] Individuals should be aware that dealing with herds of animals, should be done extremely carefully as Tinea Barabae will be contagious to other animals and spread rapidly.[3] If infection is revealed early go seek medical assistance as soon as possible.[3]
References
- 1 2 James, William D.; Berger, Timothy G.; et al. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. ISBN 0-7216-2921-0.
- ↑ Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. p. 518. ISBN 1-4160-2999-0.
- 1 2 3 4 5 6 7 Rutecki; Wurtz & Thomson (2000). "From Animal to Man: Tinea Barbae" (PDF). Retrieved 5 December 2016.
- ↑ "Ringworm, Beard (Tinea Barbae) in Adults: Condition, Treatment and Pictures - Overview". skinsight.com. Retrieved 2016-05-17.
- 1 2 3 4 5 6 7 8 "Tinea Barbae". dermnetnz.org. DermNet NZ. 2003. Retrieved 5 December 2016.
